Early Signs of AFLD to Watch For

The Subtle Warnings Your Liver Might Be Sending
Alcoholic fatty liver disease (AFLD) is a progressive condition that often starts silently, making early detection challenging but crucial. Recognizing the early signs of AFLD to watch for could mean the difference between a reversible condition and one that progresses to irreversible damage. From subtle fatigue to vague abdominal discomfort, these signs often whisper rather than shout, but as a medical professional, I’ll guide you through the critical details to identify and address them effectively.
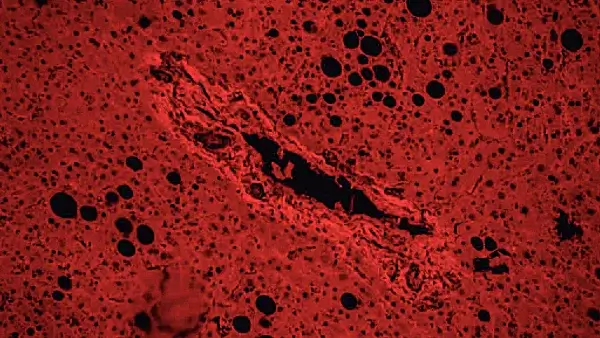
Understanding the Impact of Alcohol on the Liver
The liver serves as the body’s main detoxification organ, metabolizing alcohol and other substances. When alcohol consumption surpasses the liver’s capacity, fat begins to accumulate in liver cells. This marks the onset of AFLD. While it may remain asymptomatic in the early stages, damage compounds over time, potentially leading to inflammation, scarring, and cirrhosis if left untreated.
Fatigue and General Malaise
One of the earliest indicators of AFLD is persistent fatigue. This symptom is often dismissed as a result of a busy schedule, poor sleep, or stress. However, in individuals who drink regularly, unexplained lethargy can signal liver dysfunction. Fatigue occurs because the liver struggles to perform its usual metabolic tasks, leaving the body energy-depleted.
Accompanying this might be a sense of malaise, a general feeling of being unwell without a specific cause. Patients often describe it as a nagging “off” feeling, difficult to pinpoint but hard to ignore.
Discomfort in the Upper Right Abdomen
Another common early sign of AFLD is mild discomfort or pain in the upper right abdomen, where the liver resides. This sensation might range from a dull ache to intermittent twinges, usually noticed after meals or alcohol consumption.
Such discomfort occurs because the liver becomes enlarged as fat accumulates. Though not severe, this sign warrants further medical evaluation, particularly in individuals with regular alcohol use.
Changes in Appetite and Digestion
Early AFLD can subtly interfere with digestion. Patients may notice:
- Reduced Appetite: The desire to eat diminishes, leading to unintended weight loss.
- Nausea: A sense of queasiness after meals or alcohol consumption.
- Bloating: Discomfort caused by poor liver function affecting digestion.
While these symptoms are non-specific and overlap with other gastrointestinal conditions, they should not be ignored in the context of regular drinking.
Jaundice: A Yellowish Warning
Though typically a sign of advanced liver disease, jaundice can appear in the early stages of AFLD in some cases. This yellowing of the skin and eyes occurs when bilirubin, a byproduct of red blood cell breakdown, builds up in the blood. Even slight discoloration should prompt immediate medical attention, as it indicates liver strain.
Recognizing Ablaut Reduplication in Symptoms
Medical observations often rely on patterns, and sometimes patients report sensations that seem repetitive but escalate, such as “rumble and grumble” sensations in the stomach or “twinge and tingle” feelings in the abdomen. These descriptions, while informal, can offer valuable insights when identifying early signs of Acute Fatty Liver Disease (AFLD).
In the context of AFLD, recognizing these subtle symptoms is crucial for timely intervention. The liver's health can be compromised by various factors, including metabolic disturbances that manifest through unique sensory experiences. By paying attention to how patients articulate their discomfort—using phrases that reflect ablaut reduplication—healthcare providers can gather important clues about the underlying issues.
For instance, when a patient describes their symptoms in a repetitive manner, it may indicate a pattern of distress that warrants further investigation. This approach not only aids in diagnosis but also fosters a deeper understanding of the patient's experience, allowing for more personalized care.
Early Signs of AFLD to Watch For: Who’s Most at Risk?
While anyone consuming excessive alcohol can develop AFLD, certain groups are more susceptible:
- Women: Due to slower alcohol metabolism, women are at a higher risk of liver damage even with lower consumption.
- Individuals with Obesity: Excess body fat amplifies the risk of fat accumulation in the liver.
- Those with Genetic Predisposition: Certain genetic markers can make individuals more vulnerable.
Diagnosing AFLD: The Role of Screening
Because early AFLD symptoms can be vague, routine screening is essential for individuals at risk. Diagnostic tools include:
- Blood Tests: Elevated liver enzymes like ALT and AST can signal liver stress.
- Imaging Studies: Ultrasound or CT scans reveal fatty deposits in the liver.
- Liver Biopsy: In uncertain cases, a biopsy provides definitive confirmation.
Prevention: Intervening Early
Understanding the early signs of AFLD to watch for is only part of the equation. Equally important is taking steps to prevent or halt disease progression. Key strategies include:
- Reducing Alcohol Consumption: Limiting intake to within recommended guidelines (no more than one drink per day for women and two for men) significantly lowers risk.
- Maintaining a Healthy Weight: Shedding excess pounds through balanced nutrition and exercise reduces liver fat accumulation.
- Monitoring Liver Health: Regular liver function tests provide early warnings of damage.
Real-Life Scenario: A Patient’s Journey
Consider a 38-year-old man with a history of weekend binge drinking. He visits his physician complaining of persistent fatigue, occasional nausea, and a dull ache in his upper right abdomen. Blood tests reveal elevated liver enzymes, and an ultrasound confirms fatty infiltration of the liver.
With a diagnosis of early AFLD, the patient is advised to stop drinking immediately, adopt a liver-friendly diet, and begin a regular exercise routine. Within six months, his liver function normalizes, demonstrating that early intervention can reverse damage.
When to Seek Medical Advice
If you or someone you know drinks regularly and experiences symptoms like fatigue, abdominal discomfort, or appetite changes, seek medical advice promptly. Even mild signs can indicate underlying liver stress. Early detection allows for lifestyle changes that can prevent progression to more severe liver disease.
The Path Forward
Alcoholic fatty liver disease doesn’t develop overnight, but its progression can be insidious. By recognizing the early signs of AFLD to watch for, you can take proactive steps to protect liver health. Listen to your body, pay attention to subtle changes, and consult a healthcare professional at the first sign of trouble.
Share this article

Dr. Alinda Mae Gordola, MD
I am a board-certified internist and gastroenterologist specializing in the diagnosis and treatment of digestive system disorders. See Full Bio.
-
1. European Association for the Study of the Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012. [DOI]
-
2. Trimble G, Zheng L, Mishra A, Kalwaney S, Mir HM, Younossi ZM. Mortality associated with alcohol-related liver disease. Aliment Pharmacol Ther. 2013.
-
3. Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004.
-
4. Crabb DW. Pathogenesis of alcoholic liver disease: newer mechanisms of injury. Keio J Med. 1999.
-
5. Teli MR, Day CP, Burt AD, Bennett MK, James OF. Determinants of progression to cirrhosis or fibrosis in pure alcoholic fatty liver. Lancet. 1995.
-
6. Anstee QM, Daly AK, Day CP. Genetics of alcoholic and nonalcoholic fatty liver disease. Semin Liver Dis. 2011.
How Much Alcohol Causes AFLD? Alcoholic fatty liver disease (AFLD) is often the first stage of alcohol-induced liver damage, marked by the buildup of...
Fatty Liver Disease Prevention Risk Calculator Fatty liver disease has emerged as a silent epidemic in modern society, affecting millions of people worldwide.
Mastering Lifestyle for Fatty Liver Health The ping-pong match between one of my patients and his health had been ongoing for years. A software engineer...

You might enjoy more articles by
Dr. Alinda Mae Gordola, MD
 Disease
Disease Diets
Diets Recipes
Recipes Supplements
Supplements Management
Management Calculators
Calculators Quizzes
Quizzes Glossary
Glossary