How to Diagnose Lipodystrophy-Associated Fatty Liver

Unlocking the Mystery of Lipodystrophy-Related Liver Disease
Lipodystrophy-associated fatty liver disease is a complex condition that requires a multi-layered diagnostic approach. Understanding how to diagnose lipodystrophy-associated fatty liver involves recognizing telltale signs, utilizing precise testing methods, and identifying underlying genetic factors. This guide outlines the essential steps for accurate diagnosis to help medical professionals navigate this challenging condition.
What Is Lipodystrophy-Associated Fatty Liver?
Lipodystrophy is characterized by the abnormal or complete loss of adipose tissue, which disrupts fat storage and distribution in the body. This dysfunction often leads to excess fat being deposited in non-adipose tissues like the liver. The resulting fatty liver disease can progress silently, leading to inflammation, scarring, and even cirrhosis if left untreated.
Recognizing Clinical Indicators
A diagnosis of lipodystrophy-associated fatty liver often begins with a thorough evaluation of clinical indicators. Patients with this condition typically exhibit the following signs:
- Fat Redistribution Patterns:
The hallmark of lipodystrophy is abnormal fat loss from areas like the limbs or face, coupled with fat accumulation in other regions such as the neck or liver. - Insulin Resistance and Diabetes:
Many patients present with early-onset insulin resistance or type 2 diabetes due to disrupted fat metabolism. - Hypertriglyceridemia:
Elevated triglycerides are a frequent finding and can indicate lipid mismanagement. - Hepatomegaly:
An enlarged liver, often detected during a physical exam, suggests fat buildup or inflammation.
These features are the starting point for further diagnostic exploration.
Laboratory Tests: A Crucial First Step
Laboratory investigations are indispensable in diagnosing lipodystrophy-associated fatty liver. They offer insight into metabolic dysfunction and liver health.
- Liver Function Tests (LFTs):
Elevated levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are early indicators of liver damage. - Lipid Profile:
Abnormal lipid levels, particularly hypertriglyceridemia, are a red flag in patients with suspected lipodystrophy. - Fasting Insulin and Glucose Levels:
Elevated fasting insulin and glucose levels often suggest insulin resistance, a common complication. - Leptin Levels:
Patients with generalized lipodystrophy frequently exhibit low leptin levels due to the lack of adipose tissue.
These tests help establish the metabolic context, paving the way for targeted imaging and genetic assessments.
Imaging Techniques for Liver Assessment
Imaging plays a pivotal role in diagnosing fatty liver disease, especially when linked to lipodystrophy.
- Ultrasound:
A non-invasive and widely available tool, ultrasound can detect liver fat accumulation. However, it lacks sensitivity in early or mild cases. - Magnetic Resonance Imaging (MRI):
MRI, particularly proton density fat fraction (PDFF) analysis, offers a highly accurate assessment of hepatic fat content. - Transient Elastography (FibroScan):
This technique measures liver stiffness and helps identify fibrosis or scarring, which are common in advanced cases. - CT Scan:
While less commonly used, CT scans can quantify liver fat but expose patients to radiation.
These imaging techniques complement lab results and provide a clearer picture of the liver's health.
How to Diagnose Lipodystrophy-Associated Fatty Liver
Accurately diagnosing lipodystrophy-associated fatty liver requires synthesizing clinical, laboratory, and imaging data. The diagnostic process includes:
- Detailed Patient History:
Reviewing the patient’s medical history for signs of fat redistribution, insulin resistance, or early metabolic disorders. - Physical Examination:
Observing physical signs such as acanthosis nigricans, hepatomegaly, or regional fat loss. - Biochemical Analysis:
Utilizing lab tests to identify metabolic abnormalities and liver dysfunction. - Genetic Testing:
Genetic mutations in LMNA, PPARG, or AGPAT2 confirm specific forms of lipodystrophy. This step is crucial when a hereditary link is suspected. - Advanced Imaging:
Employing MRI or FibroScan to detect hepatic steatosis (fat accumulation) and fibrosis.
Each step builds on the last, creating a layered diagnostic approach.
Role of Genetic Testing
Genetic testing is a cornerstone in diagnosing lipodystrophy and its associated complications. Specific mutations, such as those in the LMNA gene, are closely linked to familial partial lipodystrophy (FPLD), while AGPAT2 mutations are associated with congenital generalized lipodystrophy (CGL).
These genetic insights not only confirm the diagnosis but also guide treatment strategies, such as leptin replacement therapy in severe cases.
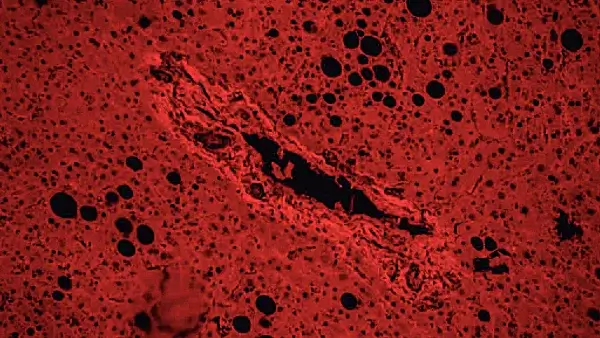
Liver Biopsy: Is It Necessary?
A liver biopsy remains the gold standard for diagnosing fatty liver disease, particularly in ambiguous or severe cases. This invasive procedure allows for direct assessment of liver tissue, identifying:
- Fat content
- Inflammation (steatohepatitis)
- Fibrosis or scarring
While highly informative, the risks of bleeding or infection mean it is reserved for cases where other diagnostic methods fail to provide clarity.
Differential Diagnoses
Not all fatty liver cases stem from lipodystrophy. Other conditions to consider include:
- Nonalcoholic Fatty Liver Disease (NAFLD):
Common in patients with obesity or metabolic syndrome. - Alcoholic Liver Disease:
Fat accumulation due to chronic alcohol consumption. - Viral Hepatitis:
Can mimic fatty liver symptoms but involves distinct pathological mechanisms.
Distinguishing lipodystrophy-associated fatty liver from these conditions is critical for appropriate treatment.
Comprehensive Management
While diagnosis is crucial, addressing the underlying causes and complications of lipodystrophy-associated fatty liver is equally important. Management includes:
- Dietary Interventions: A high-fiber, low-fat diet to reduce hepatic fat accumulation.
- Medications: Use of insulin sensitizers like metformin and lipid-lowering agents.
- Lifestyle Changes: Encouraging regular, moderate-intensity exercise.
- Hormonal Therapies: Leptin replacement therapy for patients with severe leptin deficiency.
Monitoring liver function and metabolic markers over time ensures timely adjustments to the treatment plan.
Challenges in Diagnosis
Diagnosing lipodystrophy-associated fatty liver can be challenging due to its rarity and overlapping features with other metabolic conditions. Early detection is often missed unless a comprehensive approach is taken.
Additionally, genetic testing, though valuable, may not be accessible in all healthcare settings, limiting diagnostic precision.
The Future of Diagnosis
Advances in diagnostic technology and genetic research offer hope for more precise and less invasive methods. Emerging tools include:
- Liquid Biopsies:
Detecting liver-specific biomarkers in blood samples. - Artificial Intelligence (AI):
AI-driven imaging analysis to identify subtle patterns of liver fat and fibrosis. - Next-Generation Sequencing (NGS):
Enhanced genetic testing to identify rare mutations with greater accuracy.
These innovations promise to streamline diagnosis, enabling earlier intervention and improved patient outcomes.
Conclusion
Understanding how to diagnose lipodystrophy-associated fatty liver involves a meticulous, step-by-step approach that combines clinical acumen with advanced diagnostic tools. Early recognition and intervention are critical to preventing long-term complications, such as cirrhosis or liver failure. Continued research and technological advancements will undoubtedly improve the diagnostic process, ensuring better care for affected individuals.
Share this article

Dr. Nico Pajes, MD
Dr. Nico Pajes is a board-certified internist and gastroenterologist with a focus on digestive health and internal medicine. See Full Bio.
-
1. Safar Zadeh E, Lungu AO, Cochran EK, Brown RJ, Ghany MG, Heller T, Kleiner DE, Gorden P. The liver diseases of lipodystrophy: the long-term effect of leptin treatment. J Hepatol, 2013. [DOI]
-
2. Payne F, Lim K, Girousse A, Brown RJ, Kory N, Robbins A, Xue Y, Sleigh A, Cochran E, Adams C, Dev Borman A, Russel-Jones D, Gorden P, Semple RK, Saudek V, O’Rahilly S, Walther TC, Barroso I, Savage DB. Mutations disrupting the Kennedy phosphatidylcholine pathway in humans with congenital lipodystrophy and fatty liver disease. Proc Natl Acad Sci USA, 2014.
-
3. G. Marchesini et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology, 2003.
-
4. J.L. Chan et al. Clinical effects of long-term metreleptin treatment in patients with lipodystrophy. Endocr Pract, 2011.
-
5. Guillin-Amarelle C, Sanchez-Iglesias S, Castro-Pais A, Rodriguez-Canete L, Ordonez-Mayan L, Pazos M, Gonzalez-Mendez B, Rodriguez-Garcia S, Casanueva FF, Fernandez-Marmiesse A, Araujo-Vilar D. Type 1 familial partial lipodystrophy: understanding the Kobberling syndrome. Endocrine, 2016.
-
6. C.P. Day et al. Steatohepatitis: a tale of two “hits”? Gastroenterology, 1998.
Symptoms of Lipodystrophy-Associated Fatty Liver Disease Understanding the symptoms of lipodystrophy-associated fatty liver disease is critical for...
Fatty Liver Disease Prevention Risk Calculator Fatty liver disease has emerged as a silent epidemic in modern society, affecting millions of people worldwide.
Fatty Liver IQ Quiz Understanding fatty liver disease is essential for maintaining liver health. This interactive Fatty Liver IQ Quiz helps you test your...

You might enjoy more articles by
Dr. Nico Pajes, MD
 Disease
Disease Diets
Diets Recipes
Recipes Supplements
Supplements Management
Management Calculators
Calculators Quizzes
Quizzes Glossary
Glossary